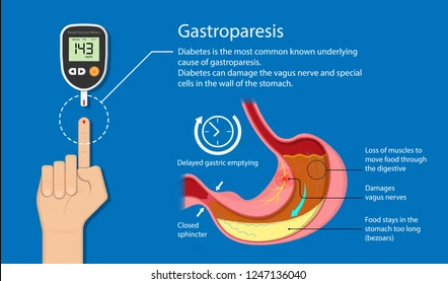
Diabetic gastroparesis is a complication that affects people with type 1 diabetes and to a more inferior extent those with type 2. It is manifested by a stomach problem, which can no longer empty its contents and so the passage of food through it is slowed down.
Gastroparesis is a type of neuropathy that affects the vagus nerve of the stomach. This nerve controls the circulation of food through the digestive tract.
If the vagus nerve is damaged, the muscles of the stomach and intestines no longer function normally, and the transition of food through the stomach is slowed or stopped.
As with other types of neuropathy, diabetes can damage the vagus nerve if blood glucose levels remain high for a long time. High blood glucose causes chemical changes in the nerves, and on the other hand causes damage to blood vessels that carry oxygen and nutrients to the nerves.
Diabetic gastroparesis symptoms
The symptoms can be mild or severe, depending on each person, metabolism, lifestyle, a period of diabetes, etc. The signs and symptoms of gastroparesis are easily recognizable, and include:
- Stomach burns
- Weight loss
- Nausea
- Vomiting in which undigested food is seen
- Abdominal bloating
- Gastroesophageal reflux
- Irregular blood sugar
- Feeling satiated at the beginning of the meal, before eating, or after eating very little
- Lack of appetite
- Stomach spasms
Gastroparesis can also make diabetes worse, because in the absence of proper digestion, blood glucose will be varied and difficult to manage. Foods that are late to be digested upset the entire glucose absorption system, with all the insulin taken.
Moreover, if the food stays in the stomach for too long, it can cause other problems, such as a bacterial superinfection, as the food begins to ferment. Also, food can harden, forming compact masses of food that can cause nausea, vomiting, and stomach obstruction. It can be dangerous if they block the passage to the small intestine.
Diagnosis
The diagnosis of diabetic gastroparesis is confirmed by performing one or more tests:
- Digestive ultrasound – With its help the doctor will be able to see if there is no other problem, such as pancreatitis or a gallbladder problem.
- Superior endoscopy – A digestive endoscopy is performed, by inserting a tube on the neck, with a video camera mounted at the end. This camera will send images inside the gastric tube, facilitating the diagnosis and showing if it is not a completely different problem. The intervention is unpleasant, so you will be easily sedated. An upper endoscopy may show that there are other causes besides diabetes for stomach problems.
- Barium radiography – After not eating anything for 12 hours, you will drink a liquid that contains barium, a slightly radioactive substance. It envelops the inside of the stomach so that it can be seen on an X-ray. In a person with a healthy stomach, after 12 hours of fasting, food is completely emptied of the intestines. If the x-ray shows that there are still undigested foods in the stomach, it is most likely gastroparesis. If the stomach is seen to be empty, but the doctor still suspects a delayed emptying of the stomach, he may tell you to repeat the test.
It is very possible to have gastroparesis but, one day, for some reason, to digest a meal normally. If you have diabetes, your doctor will tell you what to do so that the 12 hours of fasting do not affect you. - Gastric emptying scintigraphy – You will ingest a small number of foods that contain radioisotopes. By tracking the movement of radioisotopes with a device that detects their movement, the doctor will be able to check how fast food passes through the stomach. The diagnosis of gastroparesis is made if more than half of the food remains in the stomach after two hours. However, the doctor will check once every 1, 3, and 4 hours, to evaluate the rhythm of the food passing through the stomach.
- Gastric manometry – This test measures the electrical and muscular activity in the stomach. You can use electrodes placed on the skin or a thin tube that is inserted into the neck, into the stomach. The tube contains a wire that measures electrical and muscle activity while digesting liquids and solid foods. The measurements will show if the stomach is working and if there is no delay in digesting foods.
- Blood Tests – Your doctor may also recommend laboratory tests for a blood count and to measure the chemical and electrolyte levels in your stomach.
Diabetic gastroparesis treatment
In most cases, treatment does not cure diabetic gastroparesis, which is usually a chronic condition. But treatment can help to manage gastroparesis, so that you can have a functional life and as comfortable as possible.
The most important goal is to keep your blood glucose levels within normal parameters in your treatment for diabetes. You already know that if you make your insulin on time and depending on the context and be careful what you eat, you can do this, but gastroparesis can upset any observations and figures you were used to until now.
This is because food is absorbed more slowly and sometimes unpredictably. To better manage your blood glucose, your doctor will give you a specific medication, recommend that you check your blood glucose level as often as possible after eating, and will probably suggest that you try to change the frequency or timing of your blood glucose. insulin, obviously telling you exactly how.
Changing eating habits can help control gastroparesis. Talk to a diabetes nutritionist who will recommend special measures for you and the following:
- Eat six smaller meals a day instead of three large meals.
- Eat slowly, chewing well, sitting at the table.
- Take a walk after dinner, do not go straight to bed.
- Avoid foods high in fat and dietary fiber. Fats slow down digestion naturally. On the other hand, although fiber is known to aid digestion, it is difficult to digest if you do not drink enough water – they can harden and clump together.
Depending on the severity of the condition, your doctor may even recommend liquid meals or prescribe medications that help speed up digestion.
If other approaches do not work, surgery may be needed to insert a feeding tube into the stomach. The tube is inserted through the skin of the abdomen into the small intestine. It will allow the introduction of nutrients directly into the small intestine, bypassing the stomach completely. You will receive special, liquid food to use. In cases of diabetes, this may be the only solution to regulate blood glucose levels so that it reaches the bloodstream. The tube may be temporary.